You log onto the app and are waiting in the “lobby”
You finally enter the video chat with the doctor.
You tell them that you “are having a hard time breathing”
The doctor asks you “can you take a full breath”
You answer “yes, but it hurts…”
Without trying to freak you out your doctor tells you to “go to the nearest hospital!”
You’re thinking that you were just going to get some antibiotics and be on your merry way, but the concern on their face is scaring you.
“You might have a pulmonary embolism…it’s a very serious condition.”
You ask “what is a pulmonary embolism?”
They reply “it is when you have a blood clot in your lungs and it can be deadly.”
Now you’re hyperventilating and wondering if you are having a heart attack.
You are thinking should you wait, call the ambulance, or leave now?!?!
They sounded worried on the call.
The closest hospital is an hour away.
If you call the ambulance it will take a half hour to get here and then 45 mins to the hospital if they’re going pedal to the medal.
So you grab your keys and get in the car. If you die on the way then that's the way you go out.
The new normal?
This scenario is unfortunately looking to be the new normal in our communities. This report from Becker’s released in January of 2023 reports that 631 rural hospitals are at risk of closure. Hawaii is at risk of losing 75% of its hospitals. Ok, Hawaii is small you say ok let's look at Texas which is at risk of closing 50% of its hospitals. That is a staggering amount of hospitals at risk.
A couple of reasons are pinpointed why rural hospitals are particularly susceptible to closure. As we all know in the end it is usually money. As you can see in the chart below small rural hospitals don’t have the luxury of relying on private insurance reimbursements.
If you have ever worked in healthcare you know that private insurance pays out the most. Running a hospital for the rural population is a catch-22. You have to stay open 24/7 to be able to provide care for your community. So your administration costs are on par with urban hospitals but your services are not utilized as much. When they are utilized they do not make as much for those services rendered based on the makeup of the population they serve. Rural hospitals are largely propped up by grants and subsidies. They estimate that it would cost $4 billion annually to prevent these hospitals at risk from closing. That is a sizable amount but when you think that the United States spends more the $4 Trillion a year on health care it doesn’t seem too much at all.
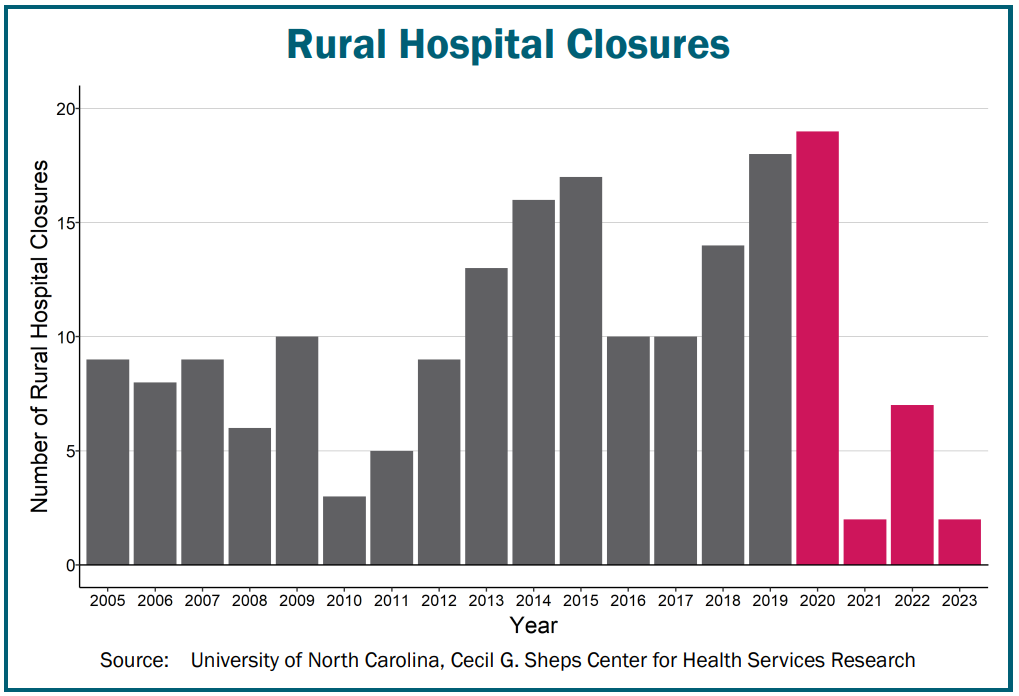
The thing is the closure of rural hospitals is not a recent phenomenon.
HOT TAKE INCOMING…
Contrary to popular belief. The pandemic didn’t make the problems worse it only shined a very bright light onto the many problems that already existed. It was only a surprise because no one was looking.
Below is a graph showing the number of rural hospital closures per year since 2005. You can see that there wasn’t a spike in hospital closures during the pandemic. It was merely continuing the trend.
Buckle up…the numbers are just beginning…
In 2018 Pew Research looks at how far Americans live from the closest hospital based on their community. They separated the communities into 3 categories which were rural, suburban, and urban. To no one's surprise, they found that people who lived in rural areas had the longest commute averaging out to 17 mins. 25% of people in rural areas lived on average 34 minutes away.
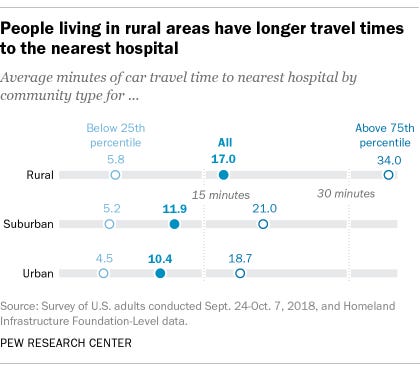
Maybe you’re thinking that‘s not too bad…🫠
The problem gets worse for people that live in areas that had a hospital close. The U.S Government Accountability Office (GAO) looked at this and they found that on average in 2018 residents had to travel on average of 24.2 miles to get to an emergency department. 35.1 miles to get to a facility with a Coronary care unit! This is where you would need to go if you were having a heart attack.
Think about that for a little bit. You’re having a heart attack and now you have a 35-mile drive ahead of you. To put that into perspective the “door to needle time” recommended by the American Heart Association is 90 minutes. That means if a patient comes in with a heart attack you need to get them into the procedure within 90 minutes of arrival. Well, good thing you had to drive almost 40 minutes to get to the hospital right?
Where am I going with all of this?
There is a lot of talk about increasing access to care with Telehealth, RPM, etc. which is great. But what happens when you’re told you are having a heart attack? Or like the person above with the pulmonary embolism. I personally don’t know of any home Cath labs or over-the-counter “clot busters.”
We can’t lose sight that access to care does not always mean access to treatment. Whatever solution we are building needs to be able to work with the physical infrastructure that exists right now. We are dealing with someone's life. Imagine someone’s mother or daughter on the other end of the zeros and ones. It doesn’t matter how much we try we will never be able to get rid of the physical visit.
So what now?
How do we solve these problems?
Usually, I have a well-thought-out solution but this time I just don’t know. Outside of paying the $4 billion dollars a year, which we know will continue to grow every year.
What I do know is that we need to use our precious few resources wisely. If it was up to me we would rebuild everything from the ground up. That simply isn’t an option.
This is what I am trying to solve. It’s what keeps me up at night. I have seen simple ailments become death sentences for people. I have stared into the eyes of families that lost their loved ones for something completely preventable because they didn’t make it to us fast enough. This is real life.
I am optimistic about what I am seeing. People are starting to open their eyes and see our system for what it is.
I know that WE can fix this together. There are more brilliant people out there than I am and I am calling on you to join us. It is a bumpy ride but one that will reap unending rewards.
Thank you so much for your support! Please do not hesitate to reach out if you have any questions or leave a comment.
You can connect with me on LinkedIn and I am trying to be more active on Twitter. Would really appreciate a follow there!
If you enjoyed what you read join 700+ founders, investor, clinicians, and executives learning how to create better healthtech products every week!
I hope you have a great day!